
1. IBD and IBS Are the Same Thing

It’s easy to mix up IBD and IBS—after all, both impact the digestive system and sound similar. But they’re completely different conditions.
Dr. Bhattacharya explained to Medical News Today that IBS (Irritable Bowel Syndrome) is more about the way the gut and brain communicate. It causes issues like bloating, abdominal pain, diarrhea, and constipation, often triggered by stress or anxiety.
IBD, on the other hand, is an autoimmune disease. The immune system mistakenly attacks the gastrointestinal tract, causing real, often severe, inflammation and damage. Symptoms can include bloody stools, extreme fatigue, unintended weight loss, rectal pain, fevers, chills, and more.
2. Stress Causes IBD

While stress can absolutely make IBD worse or trigger flare-ups, it’s not the root cause. IBD is driven by a malfunctioning immune system, not emotional stress. Still, managing stress is crucial since it can aggravate symptoms.
3. IBD Is Linked to Certain Personality Types
This one’s a myth rooted in outdated studies. When asked if personality plays a role, Dr. Bhattacharya responded clearly: “There are none that we know about.”
4. You Can Have Both Crohn’s Disease and Ulcerative Colitis
:max_bytes(150000):strip_icc()/Health-Crohns-Ulcerative-background-light-purple-ee1300a606ed4e91a4f6100738b3a534.jpg)
Crohn’s disease and ulcerative colitis are the two primary forms of IBD—but you can’t have both. Some people may have symptoms that make diagnosis tricky at first, but over time, the disease usually clarifies itself as one or the other.
5. There Are No Treatments That Help IBD

Thankfully, that’s far from the truth. Today, there are a wide range of effective treatments available depending on the severity and type of IBD.
These include powerful biologic medications such as:
- Remicade (infliximab)
- Humira (adalimumab)
- Cimzia (certolizumab pegol)
- Simponi (golimumab)
- Entyvio (vedolizumab)
- Stelara (ustekinumab)
Plus, small molecule drugs like:
- Xeljanz (tofacitinib)
- Zeposia (ozanimod)
These medications are immunosuppressants designed to control inflammation and prevent long-term damage. Clinical trials are also continually producing new treatment options.
6. Everyone With IBD Needs Surgery
Not true anymore. While surgery was once common, today’s effective treatments have significantly reduced the number of people who need it.
Dr. Bhattacharya explained that early, aggressive treatment with immunosuppressants helps prevent complications that would otherwise require surgery. According to Crohn’s & Colitis UK, only about 15% of people with ulcerative colitis need surgery within 10 years of diagnosis—and that number continues to fall.
7. IBD Medications Shouldn’t Be Taken During Pregnancy

Most IBD medications are safe during pregnancy, and keeping the disease under control is key to a healthy pregnancy.
Dr. Bhattacharya stressed that it’s much more dangerous for the disease to flare during pregnancy than to take these medications. One important exception: methotrexate, which must be discontinued even before conception.
8. You Can Stop Medications When You Feel Better

As tempting as it is to stop medication once symptoms disappear, doctors strongly advise against it.
Stopping treatment can lead to relapse, and sometimes, the same medication may no longer work if restarted. Since there’s a limited number of medication options, it’s best to stick with what’s working to avoid burning through alternatives.
9. A Gluten-Free Diet Can Cure IBD

While a gluten-free diet helps people with celiac disease or gluten sensitivity, it doesn’t treat IBD. Dietary changes might ease symptoms, but they don’t address the underlying inflammation of IBD.
10. IBD Only Affects the Digestive System
IBD’s name might suggest it’s all about the gut, but it can impact much more. It may cause issues in other parts of the body, including the skin, eyes, joints, kidneys, lungs, and liver.
These “extraintestinal manifestations” are well-documented and can pose serious challenges, requiring a coordinated treatment approach.
11. IBD Is Curable

Unfortunately, IBD currently has no cure. But medical research is advancing rapidly, and treatments are improving all the time. There’s hope for a cure in the future, but for now, management is key.
12. People With IBD Can’t Live Normal Lives
This is one of the most harmful myths—and it’s completely false. With the right treatment and support, people with IBD can live full, active, and normal lives.
Dr. Bhattacharya confirmed: “They absolutely can. With proper medical management and, sometimes, surgeries, IBD patients can live a completely normal life.”
FAQs About IBD
Q: Is IBD genetic?
A: Genetics can play a role, but environment and immune system issues are also major factors.
Q: Can I exercise with IBD?
A: Yes! Regular physical activity can actually help with fatigue and overall well-being.
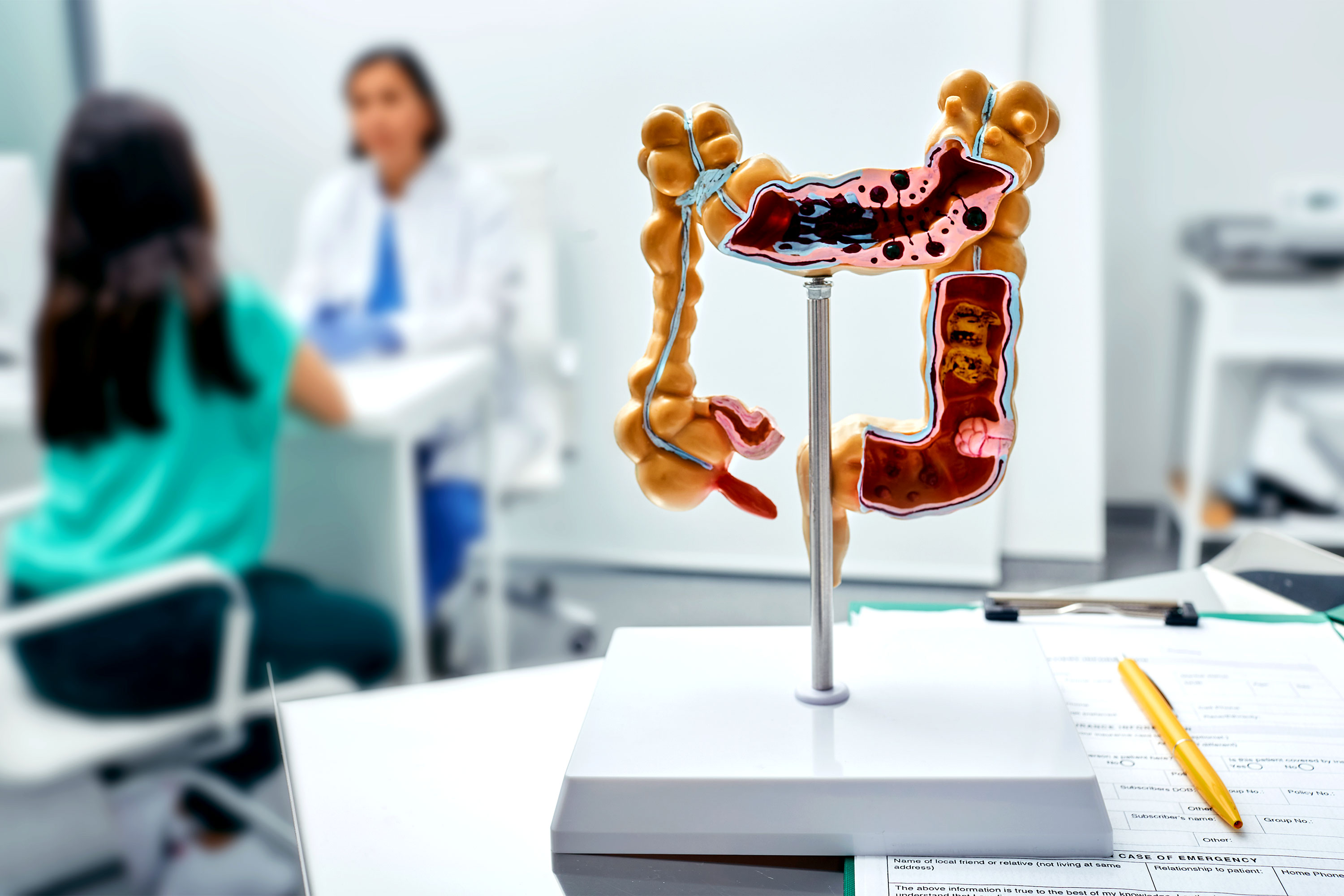
Q: How is IBD diagnosed?
A: Diagnosis usually involves blood tests, stool tests, colonoscopy, and imaging like MRI or CT scans.
Q: Is IBD contagious?
A: No, IBD is not contagious.
Q: Does diet affect IBD?
A: While no specific diet cures IBD, eating balanced, nutrient-rich food can help manage symptoms and support overall health.
Conclusion: Living with IBD
IBD can be a tough condition to manage, but today’s treatments and understanding of the disease offer real hope. Debunking myths is a powerful step toward helping people get the care, understanding, and support they deserve.
If you or someone you know is dealing with IBD, stay informed, work closely with a healthcare provider, and remember—you’re not alone, and you can live well with IBD.

